Celiac disease is estimated to impact over 3 million people in the United States. But according to the Celiac Disease Foundation, nearly 2.5 million of those people are undiagnosed. Think about it - the number of people in the United States who DON’T know they have celiac disease matches the population of the whole city of Chicago. Often, people can’t get a diagnosis until they’ve moved into a late stage of the disease, where severe intestinal damage and long-term health complications are more common. [1]
However, several other health conditions and deficiencies are connected with celiac disease and can be an early sign that something’s not right. If you’re struggling with these deficiencies, it could be worth exploring if there’s a deeper root cause.
Why does celiac disease cause nutrient deficiencies?
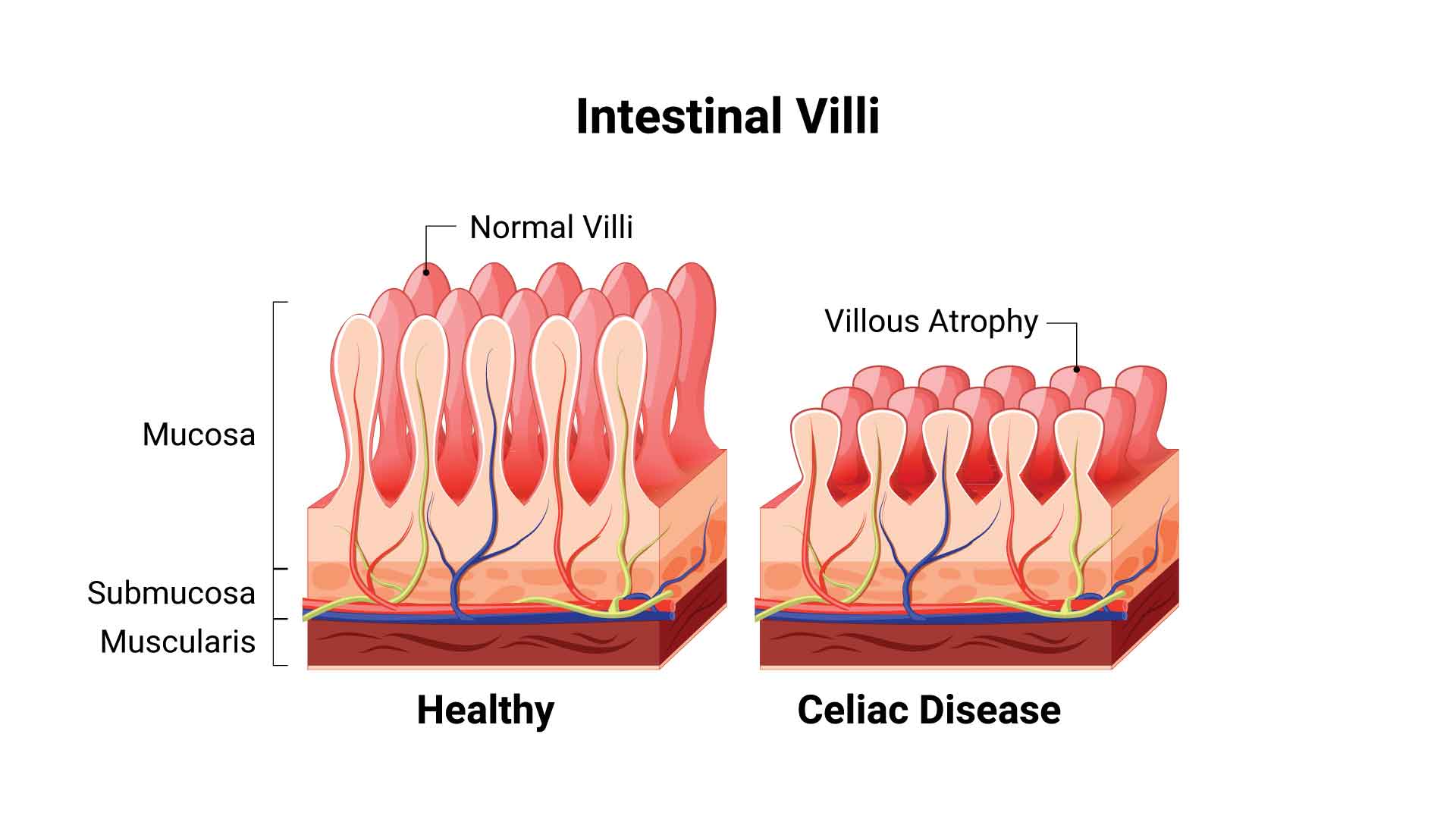
Your small intestine is full of villi, which are small, finger-like structures that are responsible for absorbing nutrients as they pass through your GI tract. When someone has celiac disease, ingesting gluten causes the immune system to attack the small intestine. Over time, the villi in the small intestine can become damaged, which makes it harder for them to absorb the nutrients it needs to function properly.
Vitamin B12 deficiency and celiac disease
Low vitamin B12 is a nutrient deficiency that has been widely associated with celiac disease. Low B12 levels can cause fatigue, weakness, heart palpitations, gastrointestinal symptoms, and nerve problems like numbness, tingling, or trouble walking.
In one small study of 39 people with celiac disease, researchers found that 41 percent of the sample size was vitamin B12 deficient. [2] However, this same study found that vitamin B12 levels returned to normal after these individuals switched to a gluten-free diet.
Low folate and celiac disease
One 2007 article noted that folic acid deficiency “continues to be a frequent finding in subjects with newly diagnosed [celiac disease] and even in adolescents and young adults with [celiac disease] detected by screening.” [3] Another 2019 study of 309 people found that the prevalence of folate deficiency was ten times higher among those with celiac disease than those without. [4]
If folate levels are low, you may experience fatigue, mouth sores, tongue swelling, and growth problems - and low folate levels in pregnant women can lead to birth defects. Folate deficiency can also lead to anemia, a condition where you have too few red blood cells.
Iron-deficiency anemia and celiac disease
Celiac disease is commonly associated with gastrointestinal symptoms such as diarrhea, bloating, gas, abdominal pain, and constipation. However, a 2007 study of 405 people found that up to 9 percent of asymptomatic patients (who weren’t having gastrointestinal problems) were diagnosed with iron-deficiency anemia. [5] A later study in 2012 found that 7 percent of those who had iron deficiency anemia (without a known cause) also had celiac disease. [6]
One 2013 study of a patient database found that, out of 727 cases, people with celiac disease that presented with anemia had more severe disease than those that presented with diarrhea. [7] If someone is suffering from anemia without a clear cause (such as trauma, pregnancy, cancer, or menstrual bleeding), doctors may do further tests to see if that person’s anemia is caused by celiac disease.

What can I do?
In many cases, nutrient deficiencies in people can be resolved with changes in diet or supplementation. But if the deficiency is rooted in your body not absorbing the nutrient properly, it’s important to address why poor absorption is happening (such as with celiac disease). In many cases, switching to a completely gluten-free diet and taking supplements can help reverse the damage, heal your small intestine, and help get rid of the deficiency.
At-home testing can be a great way to determine if you’re dealing with a nutrient deficiency so you can seek further medical guidance from your healthcare provider. Testing can also help you measure if supplements are making a difference, or determine whether you’re at risk for celiac disease in the first place.
Whether you think you have low folate, a vitamin B12 deficiency, or want to know your risk for celiac disease, an at-home test from empowerDX can help you get answers.
Sources
[1] “What Is Celiac Disease?” Celiac Disease Foundation, celiac.org/about-celiac-disease/what-is-celiac-disease/.
[2] Dahele, Anna, and Subrata Ghosh. “Vitamin B12 Deficiency in Untreated Celiac Disease.” The American Journal of Gastroenterology, vol. 96, no. 3, Mar. 2001, pp. 745–750., doi:10.1111/j.1572-0241.2001.03616.x.
[3] Halfdanarson, Thorvardur R., et al. “Hematologic Manifestations of Celiac Disease.” Blood, vol. 109, no. 2, 14 Sept. 2006, pp. 412–421., doi:10.1182/blood-2006-07-031104.
[4] Bledsoe, Adam C., et al. “Micronutrient Deficiencies Are Common in Contemporary Celiac Disease despite Lack of Overt Malabsorption Symptoms.” Mayo Clinic Proceedings, vol. 94, no. 7, 25 June 2019, pp. 1253–1260., doi:10.1016/j.mayocp.2018.11.036.
[5] Harper, Jason W., et al. “Anemia in Celiac Disease Is Multifactorial in Etiology.” American Journal of Hematology, vol. 82, no. 11, Nov. 2007, pp. 996–1000., doi:10.1002/ajh.20996.
[6] Cekin, Ayhan Hilmi, et al. “Celiac Disease Prevalence in Patients with Iron Deficiency Anemia.” The Turkish Journal of Gastroenterology, vol. 23, no. 5, 2012, pp. 490–495., doi:10.4318/tjg.2012.0467.
[7] Abu Daya, Hussein, et al. “Celiac Disease Patients Presenting with Anemia Have More Severe Disease than Those Presenting with Diarrhea.” Clinical Gastroenterology and Hepatology, vol. 11, no. 11, 10 June 2013, pp. 1472–1477., doi:10.1016/j.cgh.2013.05.030.